What Is Meningeal Syndrome?
Meningeal syndrome is a set of symptoms that appear when the meninges of the human body are affected. The causes can be varied and are life threatening. In this article, let’s see what the warning signs are and how to spot them.
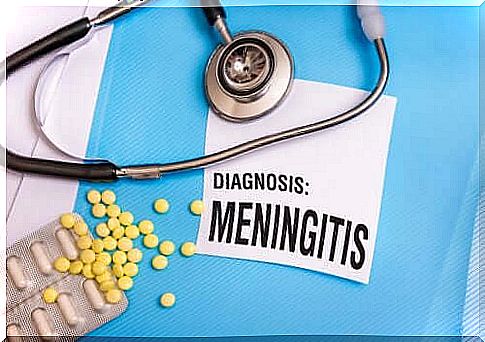
Meningeal syndrome is not a disease in itself, but rather a set of symptoms that indicate the existence of a pathological process in the meninges. The causes can be varied, but they usually require immediate attention.
In medicine, we speak of a syndrome when a group of signs and symptoms present together and are capable of responding to various etiologies. In other words, a syndrome can originate from various diseases.
In the case of meningeal syndrome, all the main symptoms are made up of three phenomena:
- Headache: headache
- Muscle stiffness: due to muscle contractures
- Fever: which may or may not be present depending on whether the origin is infectious or not
Symptoms are evident in a patient when the meninges are already inflamed. The meninges are three very thin layers that line the structures of the central nervous system inside the skull and spine. Like a kind of paper, the meninges envelop the brain and the spinal cord.
On the other hand, the meninges are three in number and are called: dura mater, pia mater and arachnoid. Meningeal syndrome responds to the last two inflammation that anatomy describes as “leptomeninges”. When these layers ignite, they irritate the central nervous system.
Causes of meningeal syndrome
Although there are various causes capable of causing meningeal syndrome, the most important fall into two groups: inflammatory and non-inflammatory. This general division does not determine the severity of the clinical case, as we will see.
Inflammatory causes
Among the inflammatory causes we can find:
- Bacteria: the most important and best known is certainly meningococcus, a microorganism for which there is a specific vaccination capable of preventing the meningitis it causes. Once the bacteria have settled in, meningeal syndrome is usually complete, with all of the symptoms. This bacteria is also capable of producing outbreaks or epidemics in populations that remain in contact. Therefore, extreme precautionary measures are taken when a case is detected and confirmed.
- Viruses: Viral meningoencephalitis has a more insidious clinical manifestation and includes relatively common viruses with rare microorganisms that cause specific diseases.
- Mycosis: the meningeal syndrome of mycotic cause is rare, but very aggressive. It usually occurs in people who have an immune deficiency and who, due to their weakened defenses, are more likely to harbor fungi. The treatment is also more complicated.
- Parasites: the parasitic meningitis is even rarer. We hardly find three microorganisms that hide behind most cases. Transmission is from animals to humans. The risk is therefore greater in the countryside.
Non-inflammatory causes
The other group of causes are the non-inflammatory ones. Among :
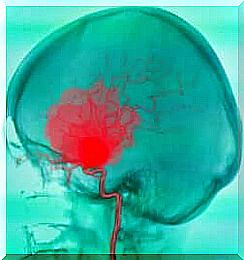
- Bleeding: When a stroke occurs as a result of a ruptured artery in the brain, the bleeding forms a pool of blood which, if near the meninges, inflames them. This then results in meningeal syndrome. At the onset of symptoms, stroke can be mistaken for bacterial meningitis, even in the presence of fever.
- Trauma: head trauma, due to blows or accidents, is capable of inflaming the meninges. Various traumatic mechanisms can actually cause the accumulation of inflammatory fluid between the brain and the leptomeninges by irritating them.
- Neoplasms: Many tumors of the brain, cerebellum and bone marrow very often begin with meningeal syndrome. The malignant mass that forms pushes on the meninges and eventually irritates them, sometimes without compressing other structures.
How to recognize a meningeal syndrome?
Since fever is not always present in meningeal syndrome, two symptoms are considered essential to recognize this phenomenon: headache and muscle contractures.
In this case, the headache is often severe and persistent pain. It is not uncommon for the patient to need to scream because of the pain in the skull. The predominant location is the forehead and occiput. In other words, at the height of the forehead or close to the nape of the neck.
This pain is usually accompanied by an intensification in the face of stimuli such as light and noise. When it intensifies with light, this is called photophobia. The person is then forced to close their eyes.
The other symptom is muscle contractures. In meningeal syndrome, the muscles in the neck, back, and lower limbs may tighten and become more rigid. The stiffness of the neck makes it impossible to bring the chin to the chest, for example. While the stiffness of the back prevents lifting the knees towards the chest. These are historical and fundamental signs that medicine has associated with meningitis for decades.
You should go to a doctor immediately if you have these symptoms. The professional will request the necessary examinations of the blood and the nervous system, up to the lumbar puncture to study the cerebrospinal fluid if necessary. It is not a framework to be taken lightly because of the risks it entails.